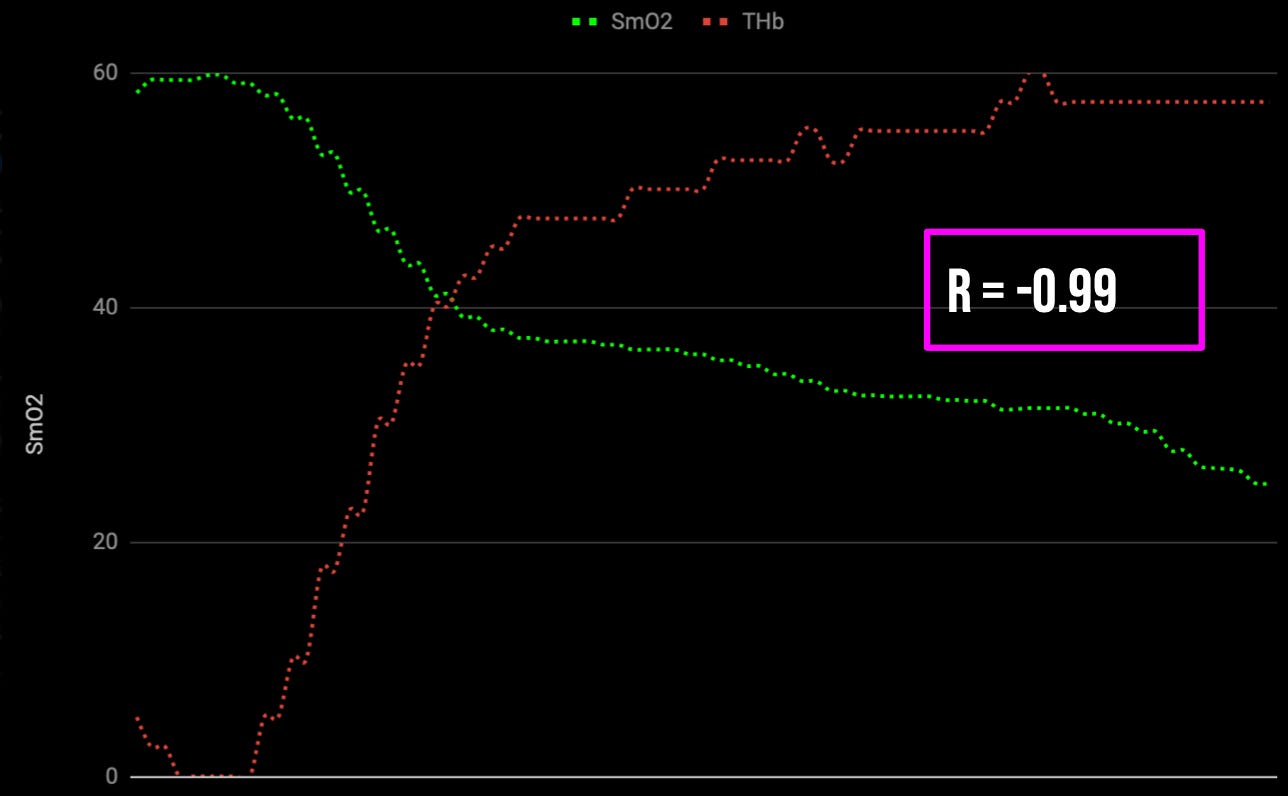
There are local feedback mechanisms in exercising muscles that respond to imbalances in oxygen supply and demand, and adjust vascular conductance which is the ease with which blood flows. This means that when muscle blood flow is compromised during exercise as is often the case during sustained high force muscle contractions, and muscle oxygen saturation levels plummet, there will be a vasodilatory response that works to restore muscle blood flow. We can observe this in the figure below, which depicts the linear relationship between muscle oxygen saturation and blood volume. For every unit of oxygen consumed, there is a proportionate compensatory increase in muscle blood flow.
However, while this response occurs under ideal scenari…
Keep reading with a 7-day free trial
Subscribe to On Human Performance by Evan Peikon to keep reading this post and get 7 days of free access to the full post archives.